|
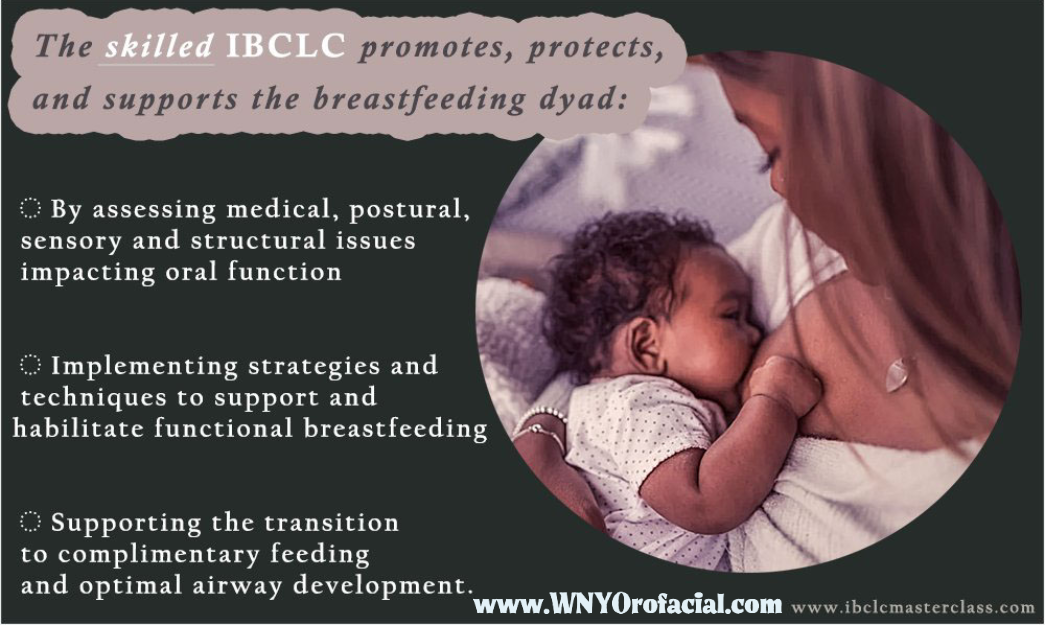
At WNY Orofacial, we are crazy about providing evidence-based, individualized care tailored for your family's particular needs. This means we assess every baby from head to toe, take an extensive medical and feeding history of the baby as well as the rest of the family, and create an individualized treatment plan that targets the root of your baby's challenges while also supporting parents to meet their feeding goals. This also includes the habilitation of your baby's oral function.
0 Comments
Birth and breast/chest feeding have been a part of history since the dawn of mammalian existence, bringing various species of mammal together in a profoundly simple, empathetic way. After all, what nursing parent can look upon a nursing lioness without a primal, instinctive understanding of the weariness in her eyes, or give a knowing smile when she pushes an overly rambunctious cub off her nipple after they get too rowdy? The birth and feeding of our young is simply a universal experience across species of mammals throughout the world.
The longevity of our species is due to this process being incredibly efficient and it allows mammals to adapt to a plethora of sub-optimal environments. There is no doubt that the medical establishment has helped our population explode from 1 billion around the year 1800 to almost 8 billion today, just 1200 years later (Worldometer, n.d.), with the evolutionary big bang that is modern western or allopathic medicine. While there is no debate that the rise of allopathic medicine has dramatically improved maternal and infant mortality rates throughout the world, these life phases are never without risk. Due to the inherently vulnerable nature of birthing parents and their children, in 1948 the newly founded United Nations deemed these cohorts have the natural, inalienable right to specialized care and support. The nature of that care and support, however, has not been specified and as a result our species continues to face too many preventable maternal and infant deaths throughout the world. This paper will focus on the United States specifically as a relatively wealthy, developed nation as the challenges in developed nations are quite different than those in developing nations having already successfully overcome many of the challenges that developing nations continue to face regarding access to safe homes, clean water and basic medical care, for example. The first step is to come in for a head to toe assessment of your baby's orofacial function so that we can tailor an individualized treatment plan for your family. We will recommend a bodywork provider to work with you that will support the work we do to correct your baby's orofacial challenges! Craniosacral therapy (CST) is the best treatment modality we have available in Western NY, and is different than chiropractic (while every CST around here is also a chiro, not all chiros are CSTs). We're fortunate to have a network of fabulous bodyworkers in the region that we work very closely with to ensure that your baby can suck, swallow, and breathe appropriately to support their future development. In the event that your baby needs further treatment for their tethered oral tissues, such as a surgical tongue/lip/cheek release, we will not just refer you for treatment but we will attend that appointment with you and even assist in the procedure so you can rest assured that your baby's care will be provided by someone you've already built a trusting relationship with who is truly invested in your baby's success. For functional development of the mouth, lips, and cheeks, you want to have a specialist helping you and your baby. WNY Orofacial is the only specialty provider on this side of Syracuse for tongue, lip, and cheek ties and other orofacial dysfunction. When Zeus sought divinity for his son Hercules, born of an adulterous affair with the mortal Alcmene, he sneaked the infant into the bedroom of his sleeping wife, Hera, and put him to her breast for a taste of infinity… Hercules suckled so hard that Hera awoke, and she shook him off in outrage, spurting milk across the skies- hence the Milky Way. Hercules already had swallowed enough, though, to join the ranks of the immortals. Reproductive Justice
It is customary practice for healthcare professionals to obtain consent for treatment from their patients. Of course, this assumes that the professionals deem their patient capable of consent. In the case of obstetricians, many consider the fetus to be their patient at least as equally as the mother. Some states grant rights and protections to the fetus that is denied to the mother in the face of a disagreement or refusal to consent to procedures the healthcare professional deems in the best interest of the fetus, even if there is a risk posed to the mother. Even if the mother does consent to a procedure that puts her at risk, such as a surgical birth called a cesarean or c-section, consent is not as simple to obtain as it may initially appear. The mere fact that a person provides written consent for a medical procedure is not necessarily indicative of an autonomous decision, especially when she may be agreeing to submit to someone in a perceived position of authority such as her physician, or to circumstances beyond her control (Roberts, 1997). Especially in the case of a poor parent or a parent of color, there are certainly plenty of reasons to be wary of causing waves within the medical establishment. The evidence supports this, as discriminatory enforcement of child endangerment laws are well-documented especially among black parents at a rate ten times higher than white parents (Roberts, 1997). In 2004, Melissa Rowland initially refused a cesarean birth for her twins at one hospital, choosing instead to have her cesarean at a different hospital a week and a half later. After one of her fetuses was born a daughter whose blood was positive for both cocaine and alcohol, and the other a stillborn son, the District Attorney’s office charged her under a state statute which established her deceased fetus “as a person for the purposes of criminal prosecution and a theory of conduct evincing a depraved indifference to the value of human life” (Wilde, 2004) and child endangerment. She later accepted a plea deal dropping the homicide charge and pleading guilty to two charges of child endangerment for her use of cocaine during her pregnancy, losing custody of her daughter in the process (Miller, 2005). Eugenics is understood as a movement in the early 20th century intended to improve human heredity. On its face, the movement is a noble one, concerned that public policies to improve the lives of the weakest of our species (which they defined as the mentally ill, disabled, and degenerate) were dramatically influencing the Darwinian evolution of the human race in such a way that might lead to the inferiority of our species. It was on the movement’s influence upon the accepted public discourse and integration within government bodies that led to some of the century’s most heinous legislation, resulting in the loss of bodily choice and integrity for many of our nation’s most marginalized and therefore vulnerable individuals. The very terms segregation and sterilization were originally used in eugenic and bacteriologist literature to mean selective isolation or quarantine and “to eliminate the agents that reproduced disease,” respectively, prior to their use in more recent common vernacular (Pernick, 1997, p. 1769), which implies the original intentions with which these terms were used colloquially. Ellsworth Huntingdon, scientist and one-time president of the board of directors of the American Eugenics society (Text Book History, N.D.), claimed that “America is seriously endangering her future by making fetishes of equality, democracy, and universal education (as quoted in Roberts, 1997, p. 51) by looking to care for our most vulnerable citizens. This paper will show how the aims he sought in these three areas have continued to hold strong through the last hundred years, despite decades of activists’ efforts to the contrary. There are few ways in which our lives are left untouched by way of policy. The most intimate aspects of adult lives are regulated by way of government policy and therefore our level of social privileges. Heterosexism and racism are sanctioned similarly by way of institutional mechanisms used to perpetuate both sexual and racial socioeconomic hierarchies. One such mechanism is the polarization between the binary normal (white, heterosexual, cisgender) and the deviant (person of color, LGBTQ+) that has permeated the public discourse (Nicholson-Crotty, 2005). Another has been the segregation and widening disparities between socioeconomic classes that has given rise to decrepit inner-city ghettos and underrepresented blue-collar communities (mostly filled with people of color) throughout this beautiful country (Collins, 2004).
I propose that degenerative politics are a clear ploy for the age-old villain, the wealthy white man of advanced age who shakes his fists at those “meddling kids,” otherwise known as the rights activists of the times while slyly working the political system to his personal benefit. I’ll show how time and again, political actors engage in these types of binary politics where they are the good guys while the demographic they are targeting (be they African American, poor, female, and/or LGBTQ+) is bad or somehow a threat to the American way of life. They do this to win support from their constituents by uniting them against a commonly perceived threat and also to gain political capitol in terms of alliances with other political actors in the system from within which they work. WNY Orofacial encourages an evolutionary approach to the introduction of solids foods for the breastfed baby. This closely follows the recommendations of "Baby Led Weaning," (BLW) a method of introducing solids coined by Gil Rapley, a former health visitor and midwife in the U.K. There, the term "weaning" is intended to mean the introduction of anything besides from breastmilk to the baby rather than the common US interpretation of giving up breastmilk altogether.
At what point should you introduce solid foods? Even the AAP recommends nothing before 6 months of age, and is unapologetically opposed to giving solids too early (even with physician encouragement). Giving solids too early jeopardizes the virgin gut, meaning the intestines, where the majority of our immunities are rooted, become compromised and the risk for a leaky gut arises, which can result in food allergies and autoimmune dysfunction. According to kellymom.com: Signs that indicate baby is developmentally ready for solids include:
The main difference between traditional BLW and what we recommend is the style of offering foods- rather than finger sized pieces of many foods, we encourage offering food in as whole and uncooked a form as possible- for example, a lightly blanched broccoli floret, so baby can gnaw on the end while holding a "handle," a peeled thick raw carrot, or a whole apple with a bite taken out. The idea is that the baby can taste the flavors and experience the textures without filling the tummy. Whenever this is impossible (as one wouldn't want to give a baby a nearly raw sweet potato, for example), thick, finger-like pieces may be baked and offered. As with any method of feeding, parents should always be present to supervise and should be familiar with various methods to alleviate choking in their infant. Click here to learn how to help an infant when they are choking. Also, here is some additional reading from baby center. Personally attending a training is the best way to learn! There are trainings offered periodically in the Buffalo area- please check them out! You may be asking yourself, don't they need food to provide iron after 6 months? According to Dr. Jack Newman, world renowned breastfeeding expert and pediatrician, no. In fact, he extrapolates the data to show that artificially increasing iron levels in infants may actually lead to increased incidence of illness. Read on to learn his thoughts on when solid foods should be introduced: Dr.Jack Newman - October 10 There is a lot of talk these days about having to start solids now at four months of age to "prevent allergies", apparentlly supported by "scientific research". This is a sea-change from even a couple of years ago when the idea was to start solids at six months of age. However the "scientific support" for starting solids at 4 months of age is not as interpreted. If the "scientific data" says anything, it says one can prevent allergies by starting solids at between 4 to 6-7 months, so why does this get interpreted as 4 months? I should say that the "science" is less than convincing. It is obvious that allergy is not due to just one thing (when the breastfed baby starts solids), but a host of environmental factors seem to have a role. Babies should start solids when the are developmentally ready, not by the calendar. The following is an excerpt from my recently revised book, Dr Jack Newman's Guide to breastfeeding. Babies, especially breastfed babies, are pretty amazing. It doesn't matter how long they generally sleep, they frequently wake up and want to breastfeed when the mother, but not necessarily the father, just sits down to eat. This happens even if the mother and father are not eating at the same time. How do the babies know this? Is there some sort of chemical signal that the mother sends out that says “I’m just about to put the fork into my mouth”? I suppose it’s possible. If pheromones can induce humans to be sexually attracted to each other, why not maternal pheromones that say “it’s time to eat”? There is no scientific proof for this, but the experience of mothers is important and we should listen to them more often. In any case, the result is that babies are often sitting on their mother’s or father’s lap when one or the other is eating. By about four months of age, the baby becomes very interested in what is going on. He will often watch attentively the fork or spoon the mother is using to eat as it moves back and forth from the plate to the mother’s mouth and back again. By five or six months he not only watches, he may try to grab food out of the plate and put it into their mouths. In fact, I have seen babies put their hands into the mother’s mouth to try to take the food out of her mouth. It seems to me that a baby doing this is ready to eat solids whatever his age. Of course, a two month old won’t behave like this, so there is no question, following my approach, of the baby’s being ready to eat solids at two or three months. And if the baby is ready for solids at five months and two weeks of age, why not start the baby eating solids when he’s so interested? And what solids should the baby get when he’s ready? I think it makes sense that the baby of five months and two weeks of age who is trying to grab the piece of steak out of the mother’s plate be allowed to eat that piece of steak. Okay, it can be cut to a reasonable size or shredded, but the same food as the parents eat, with only a few exceptions. Which exceptions? Round, slippery food, such as whole grapes or peanuts are not a good idea. They are often just the size to block the baby’s trachea (breathing tube). Hot dogs present a similar risk. Popcorn has been cited as a food that can be aspirated into the trachea. Also very hot spicy food may be better to avoid for a while as burning the baby’s mouth is probably not a great way to encourage him to eat solids. But that’s about all. Of course, making sure the food is not too hot (in the sense of temperature) is just common sense and not only for babies or children. There’s often no need to cut the food into small pieces: a baby can hold a broccoli floret in his hand and gnaw away at it, or pick up a pear with two hands and chomp on it. But I have heard the argument that a baby of five or six months will put anything into his mouth, even stones and toys, if he has the opportunity. Yes, this is true and since the parents are usually there when a six month old baby is putting a plastic toy into his mouth, they will usually quickly and anxiously pull the toy out of his mouth. The baby has just learned that toys are not food or at least not to be put into the mouth though they will keep trying from time to time until they really learn. I would suggest, then, that if a baby puts a piece of chicken into his mouth and the parents react in the same way to the chicken as they would to the stone, the baby has just learned that maybe chicken is not food either. Excerpted from Facebook posts that were too good to lose:
Dr.Jack Newman- September 21 · I am concerned because I have received 2 emails in 2 days where a mother of a baby (in the second case a 9 month old) has been told that “breastfeeding causes iron deficiency”. Those words exactly. According to the mother of the 9 month old baby, the baby is eating meat at least once a day, sometimes twice a day and is eating iron fortified baby cereal in the morning. That the pediatrician would put it this way, that “breastfeeding causes iron deficiency” boggles the mind. And it worries me that I have received two similar emails in two days. I hope this is a coincidence and not a new trend based on some silly article or some talk at a conference by someone who knows nothing about breastfeeding toddlers or infant nutrition for that matter. In a way a pediatrician who says this is stating that formula is somehow better than breastfeeding. The pediatrician wanted the mother to breastfeed less frequently and give more frequent feedings of solids. As if solids somehow replace breastfeeding. Even though this 9 month old’s diet seems perfectly adequate from the point of view of his getting his requirements of iron. In fact, from all points of view. This pediatrician forgets (or never realized) that breastfeeding is much more than nutrition. Breastfeeding is not just another way of getting calories and other nutrients (including iron) into a baby. Breastfeeding is not just another way of feeding a baby with a “bottle” that is softer than plastic or glass bottles but essentially the same. Aside from the nutritional point of view, breastfeeding is chock full of many types of immune protective factors (not just antibodies) and growth factors (that help the baby’s gut, brain and other systems to develop) and even stem cells. But breastfeeding is also a relationship, a close, intimate relationship between two people in love. The question of iron deficiency has reached the point almost of hysteria, supported by formula companies who keep stressing to health professionals that one of the main reasons to give formula after the first 6 months is that it is a way of making sure that babies get enough iron. Which is ridiculous as the iron in formula is artificially added, so essentially it is really equivalent to giving babies medicinal iron. And the majority of the iron in formula (and baby cereals) ends up in the baby’s diaper. One of the most frequently cited reasons for starting babies on solids is that if they don´t start eating iron rich food they will become iron deficient and this is where the notion of "breastfeeding causes iron deficiency" comes in. This is further complicated by mothers being told to "replace breastfeeding with solids". What people need to understand is the following: 1) After the baby is six months of age, solids are ADDED to breastfeeding, they do not replace breastfeeding. 2) Breastmilk does contain iron and the iron in breastmilk is very well absorbed. So babies need the iron in breastmilk and addition iron in solids. 3) Breastfeeding shouldn't be replaced by formula after the first six months. The notion that formula needs to be introduced at some point in the baby's life is wrong. Breastfed babies eating solids don't need formula ever. 4) Breastmilk is still the main source of nutrition for babies after the first 6 months because it still contains all those hundreds of nutrients, cells and factors that it contained before. Dr.Jack Newman - September 24 · As a followup to the iron issue about which I posted here on September 21, the following is the abstract of an article that was published in the journal AMERICAN JOURNAL OF HUMAN BIOLOGY 26:10–17 (2014). It questions the basic assumption of what might be "normal" for the formula fed baby should be considered normal for the breastfed baby. Here is the abstract: Recently, there has been considerable debate regarding the appropriate amount of iron fortification for commercial infant formula. Globally, there is considerable variation in formula iron content, from 4 to 12 mg iron/L. However, how much fortification is necessary is unclear. Human milk is low in iron (0.2–0.5 mg/L), with the majority of infant iron stores accumulated during gestation. Over the first few months of life, these stores are depleted in breastfeeding infants. This decline has been previously largely perceived as pathological; it may be instead an adaptive mechanism to minimize iron availability to pathogens coinciding with complementary feeding. Many of the pathogens involved in infantile illnesses require iron for growth and replication. By reducing infant iron stores at the onset of complementary feeding, infant physiology may limit its availability to these pathogens, decreasing frequency and severity of infection. This adaptive strategy for iron regulation during development is undermined by the excess dietary iron commonly found in infant formula, both the iron that can be incorporated into the body and the excess iron that will be excreted in feces. Some of this excess iron may promote the growth of pathogenic, iron requiring bacteria disrupting synergistic microflora commonly found in breastfed infants. Evolutionarily, mothers who produced milk with less iron and infants who had decreased iron stores at the time of weaning may have been more likely to survive the transition to solid foods by having limited iron available for pathogens. Contemporary fortification practices may undermine these adaptive mechanisms and increase infant illness risk. Am. J. Hum. Biol. 26:10–17, 2014. VC 2013 Wiley Periodicals, Inc. Dr.Jack Newman - September 24, 2013 · The following is from a blog by a mother who tested her milk for alcohol. Not one of those useless kits that you can buy at various stores, but tested at a toxicology laboratory. I will copy from her blog the method she used and the results. I think this puts the lie to the notion that women should not drink while breastfeeding or need to "pump and dump" (an appalling term) after having even one drink. The following is an exact quote from her blog:
Method: First I took a sample of my milk (about 1 mL) prior to drinking any alcoholic beverage. I expressed the milk mid-nursing session to ensure I had a goodly portion of fore & hind milk. After completing the nursing session, I mixed myself an alcoholic beverage consisting of 2 oz of 80 proof (40%) vodka in 10 oz of soda (Sprite). I proceeded to drink the entire 12 oz in about 30 minutes. About 30 minutes after finishing (1 hour after beginning to drink), I expressed some milk (about 1 mL) and labeled it 'immediate'. I then waited 1 hour and expressed more milk (about 1 mL) and labeled it '2 hours'. In the 2 hours (from the beginning), I did not drink any more alcoholic beverages, drink other beverages, or eat any other foods. Another day, 1/2 of a beer (4.3% alcohol) and 2-6 oz glasses of wine were consumed within 1.5 hours. About an hour from the beginning of the last drink, a milk sample (about 1 mL) was taken. This sample was labeled '1 hour - 3 drinks'. Another sample was taken about an hour after that (2 hours after the beginning of the last drink). This sample was labeled '2 hours - 3 drinks'. The samples were stored in the refrigerator until processing. An Agilent headspace instrument was used to run the tests. Propanol and ethanol standards were also tested to ensure the instrument was within limits. The instrument is maintained by the KSP Lab Toxicology Section and used in forensic determinations of blood and urine alcohol content. Results: The sample labeled as 'immediate' registered as 0.1370 mg/mL which correlates to 0.01370% alcohol in the sample. The sample labeled '2 hours' registered as 0.0000 mg/ml which correlates to 0.0000%. The sample labeled '1 hour - 3 drinks' registered as 0.3749 mg/mL which correlates to 0.03749% alcohol in the sample. The sample labeled '2 hours - 3 drinks' registered as 0.0629 mg/mL which correlates to 0.00629% alcohol in the sample. Conclusion: The alcohol content in breast milk immediately after drinking is equivalent to a 0.0274 proof beverage. That's like mixing 1 oz of 80 proof vodka (one shot) with 2919 oz of mixer . By the way, 2919 oz is over 70 liters. Two hours after drinking one (strong) drink the alcohol has disappeared from the sample. Completely harmless to the nursing infant. Drinking about 3 drinks in 1.5 hours resulted in higher numbers, but still negligible amounts of alcohol would be transferred to the child. One hour after imbibing in 3 drinks, the milk was the equivalent of 0.07498 proof beverage. That would be like adding 1 oz of 80 proof vodka (one shot) to 1066 oz of mixer (1066 oz is over 26 liters). Two hours after imbibing in 3 drinks, the milk was 0.01258 proof. That would be like adding 1 oz of 80 proof vodka to 3179 oz of mixer (over almost 80 liters). So, even though an infant has much less body weight, any of these percentage of alcohol in breast milk is unlikely to adversely affect the baby. Bottoms up! All you need is a tank or belly band underneath your shirt/sweater. Old Navy is a great place to get tanks that perfectly match your shirt, so you can easily layer in a way that doesn't draw any attention to what you're doing. People won't even know you're nursing your baby unless they get very, very close to you! This is also a great method for chilly days, so your chest/belly don't catch a chill. Happy nursing! |
Archives
March 2022
Categories
All
|
HO*LIS*TIC ~ADJECTIVE: Relating to or concerned with complete systems rather than with individual parts
WNY Orofacial & Breastfeeding Support Center is a division of Holistic Parenting Network, LLC, located within the village of East Aurora, NY.
131 Orchard Park Rd. West Seneca, NY 14224 fax: (716) 508-3302 (716) 780-2662 [text friendly]
WNY Orofacial & Breastfeeding Support Center is a division of Holistic Parenting Network, LLC, located within the village of East Aurora, NY.
131 Orchard Park Rd. West Seneca, NY 14224 fax: (716) 508-3302 (716) 780-2662 [text friendly]


 RSS Feed
RSS Feed