|
Excerpted from Facebook posts that were too good to lose:
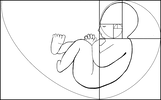
Dr.Jack Newman- September 21 · I am concerned because I have received 2 emails in 2 days where a mother of a baby (in the second case a 9 month old) has been told that “breastfeeding causes iron deficiency”. Those words exactly. According to the mother of the 9 month old baby, the baby is eating meat at least once a day, sometimes twice a day and is eating iron fortified baby cereal in the morning. That the pediatrician would put it this way, that “breastfeeding causes iron deficiency” boggles the mind. And it worries me that I have received two similar emails in two days. I hope this is a coincidence and not a new trend based on some silly article or some talk at a conference by someone who knows nothing about breastfeeding toddlers or infant nutrition for that matter. In a way a pediatrician who says this is stating that formula is somehow better than breastfeeding. The pediatrician wanted the mother to breastfeed less frequently and give more frequent feedings of solids. As if solids somehow replace breastfeeding. Even though this 9 month old’s diet seems perfectly adequate from the point of view of his getting his requirements of iron. In fact, from all points of view. This pediatrician forgets (or never realized) that breastfeeding is much more than nutrition. Breastfeeding is not just another way of getting calories and other nutrients (including iron) into a baby. Breastfeeding is not just another way of feeding a baby with a “bottle” that is softer than plastic or glass bottles but essentially the same. Aside from the nutritional point of view, breastfeeding is chock full of many types of immune protective factors (not just antibodies) and growth factors (that help the baby’s gut, brain and other systems to develop) and even stem cells. But breastfeeding is also a relationship, a close, intimate relationship between two people in love. The question of iron deficiency has reached the point almost of hysteria, supported by formula companies who keep stressing to health professionals that one of the main reasons to give formula after the first 6 months is that it is a way of making sure that babies get enough iron. Which is ridiculous as the iron in formula is artificially added, so essentially it is really equivalent to giving babies medicinal iron. And the majority of the iron in formula (and baby cereals) ends up in the baby’s diaper. One of the most frequently cited reasons for starting babies on solids is that if they don´t start eating iron rich food they will become iron deficient and this is where the notion of "breastfeeding causes iron deficiency" comes in. This is further complicated by mothers being told to "replace breastfeeding with solids". What people need to understand is the following: 1) After the baby is six months of age, solids are ADDED to breastfeeding, they do not replace breastfeeding. 2) Breastmilk does contain iron and the iron in breastmilk is very well absorbed. So babies need the iron in breastmilk and addition iron in solids. 3) Breastfeeding shouldn't be replaced by formula after the first six months. The notion that formula needs to be introduced at some point in the baby's life is wrong. Breastfed babies eating solids don't need formula ever. 4) Breastmilk is still the main source of nutrition for babies after the first 6 months because it still contains all those hundreds of nutrients, cells and factors that it contained before. Dr.Jack Newman - September 24 · As a followup to the iron issue about which I posted here on September 21, the following is the abstract of an article that was published in the journal AMERICAN JOURNAL OF HUMAN BIOLOGY 26:10–17 (2014). It questions the basic assumption of what might be "normal" for the formula fed baby should be considered normal for the breastfed baby. Here is the abstract: Recently, there has been considerable debate regarding the appropriate amount of iron fortification for commercial infant formula. Globally, there is considerable variation in formula iron content, from 4 to 12 mg iron/L. However, how much fortification is necessary is unclear. Human milk is low in iron (0.2–0.5 mg/L), with the majority of infant iron stores accumulated during gestation. Over the first few months of life, these stores are depleted in breastfeeding infants. This decline has been previously largely perceived as pathological; it may be instead an adaptive mechanism to minimize iron availability to pathogens coinciding with complementary feeding. Many of the pathogens involved in infantile illnesses require iron for growth and replication. By reducing infant iron stores at the onset of complementary feeding, infant physiology may limit its availability to these pathogens, decreasing frequency and severity of infection. This adaptive strategy for iron regulation during development is undermined by the excess dietary iron commonly found in infant formula, both the iron that can be incorporated into the body and the excess iron that will be excreted in feces. Some of this excess iron may promote the growth of pathogenic, iron requiring bacteria disrupting synergistic microflora commonly found in breastfed infants. Evolutionarily, mothers who produced milk with less iron and infants who had decreased iron stores at the time of weaning may have been more likely to survive the transition to solid foods by having limited iron available for pathogens. Contemporary fortification practices may undermine these adaptive mechanisms and increase infant illness risk. Am. J. Hum. Biol. 26:10–17, 2014. VC 2013 Wiley Periodicals, Inc.
1 Comment
|
Archives
March 2022
Categories
All
|
HO*LIS*TIC ~ADJECTIVE: Relating to or concerned with complete systems rather than with individual parts
WNY Orofacial & Breastfeeding Support Center is a division of Holistic Parenting Network, LLC, located within the village of East Aurora, NY.
131 Orchard Park Rd. West Seneca, NY 14224 fax: (716) 508-3302 (716) 780-2662 [text friendly]
WNY Orofacial & Breastfeeding Support Center is a division of Holistic Parenting Network, LLC, located within the village of East Aurora, NY.
131 Orchard Park Rd. West Seneca, NY 14224 fax: (716) 508-3302 (716) 780-2662 [text friendly]

 RSS Feed
RSS Feed