|
The first step is to get bodywork for your baby. Craniosacral therapy (CST) is the best treatment we have available in Western NY, and is different than chiropractic (while every CST around here is also a chiro, not all chiros are CSTs). Dr Michelle Pietrantone (with whom we share an office) is a fabulous one, but unfortunately she's not taking new patients at this time. Dr Alaina Ferry at Infinite Health Chiropractic, Dr Alaina Roswell at Riverview Chiropractic, and Dr Jessica Przbylak from Family Chiropractic are the only providers in the region for CST as far as I'm aware, but I'm always happy to chat with providers who may offer this service, so please reach out to us if you'd like to discuss working together!
Dairy allergies are being diagnosed at a terrifying rate in our area, and without testing. Blood in the stool is pretty common (close to 70% of babies experience this at some point) and is not a sign of allergy. It is a sign of intestinal inflammation. The best treatment is to address the inflammation and fix the problem, rather than to just avoid foods you normally eat, stop breastfeeding, or change formulas. WNY Orofacial & Breastfeeding Support Center can help get to the root of the problem so that you can get on with your life. For functional development of the mouth, lips, and cheeks, you want to have a specialist helping you and your baby. WNY Orofacial is the only specialty provider on this side of Syracuse for tongue, lip, and cheek ties and other orofacial dysfunction.
0 Comments
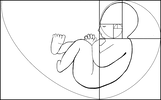
The Breastfeeding Support Center of WNY encourages an evolutionary approach to the introduction of solids foods for the breastfed baby. This closely follows the recommendations of "Baby Led Weaning," (BLW) a method of introducing solids coined by Gil Rapley, a former health visitor and midwife in the U.K. There, the term "weaning" is intended to mean the introduction of anything besides from breastmilk to the baby rather than the common US interpretation of giving up breastmilk altogether. At what point should you introduce solid foods? Even the AAP recommends nothing before 6 months of age, and is unapologetically opposed to giving solids too early (even with physician encouragement). Giving solids too early jeopardizes the virgin gut, meaning the intestines, where the majority of our immunities are rooted, become compromised and the risk for a leaky gut arises, which can result in food allergies and autoimmune dysfunction. According to kellymom.com: Signs that indicate baby is developmentally ready for solids include:
The main difference between traditional BLW and what we recommend is the style of offering foods- rather than finger sized pieces of many foods, we encourage offering food in as whole and uncooked a form as possible- for example, a lightly blanched broccoli floret, so baby can gnaw on the end while holding a "handle," a peeled thick raw carrot, or a whole apple with a bite taken out. The idea is that the baby can taste the flavors and experience the textures without filling the tummy. Whenever this is impossible (as one wouldn't want to give a baby a nearly raw sweet potato, for example), thick, finger-like pieces may be baked and offered. As with any method of feeding, parents should always be present to supervise and should be familiar with various methods to alleviate choking in their infant. Click here to learn how to help an infant when they are choking. Also, here is some additional reading from baby center. Personally attending a training is the best way to learn! There are trainings offered periodically in the Buffalo area- please check them out! You may be asking yourself, don't they need food to provide iron after 6 months? According to Dr. Jack Newman, world renowned breastfeeding expert and pediatrician, no. In fact, he extrapolates the data to show that artificially increasing iron levels in infants may actually lead to increased incidence of illness. Read on to learn his thoughts on when solid foods should be introduced: Dr.Jack Newman - October 10 There is a lot of talk these days about having to start solids now at four months of age to "prevent allergies", apparentlly supported by "scientific research". This is a sea-change from even a couple of years ago when the idea was to start solids at six months of age. However the "scientific support" for starting solids at 4 months of age is not as interpreted. If the "scientific data" says anything, it says one can prevent allergies by starting solids at between 4 to 6-7 months, so why does this get interpreted as 4 months? I should say that the "science" is less than convincing. It is obvious that allergy is not due to just one thing (when the breastfed baby starts solids), but a host of environmental factors seem to have a role. Babies should start solids when the are developmentally ready, not by the calendar. The following is an excerpt from my recently revised book, Dr Jack Newman's Guide to breastfeeding.
Babies, especially breastfed babies, are pretty amazing. It doesn't matter how long they generally sleep, they frequently wake up and want to breastfeed when the mother, but not necessarily the father, just sits down to eat. This happens even if the mother and father are not eating at the same time. How do the babies know this? Is there some sort of chemical signal that the mother sends out that says “I’m just about to put the fork into my mouth”? I suppose it’s possible. If pheromones can induce humans to be sexually attracted to each other, why not maternal pheromones that say “it’s time to eat”? There is no scientific proof for this, but the experience of mothers is important and we should listen to them more often. In any case, the result is that babies are often sitting on their mother’s or father’s lap when one or the other is eating. By about four months of age, the baby becomes very interested in what is going on. He will often watch attentively the fork or spoon the mother is using to eat as it moves back and forth from the plate to the mother’s mouth and back again. By five or six months he not only watches, he may try to grab food out of the plate and put it into their mouths. In fact, I have seen babies put their hands into the mother’s mouth to try to take the food out of her mouth. It seems to me that a baby doing this is ready to eat solids whatever his age. Of course, a two month old won’t behave like this, so there is no question, following my approach, of the baby’s being ready to eat solids at two or three months. And if the baby is ready for solids at five months and two weeks of age, why not start the baby eating solids when he’s so interested? And what solids should the baby get when he’s ready? I think it makes sense that the baby of five months and two weeks of age who is trying to grab the piece of steak out of the mother’s plate be allowed to eat that piece of steak. Okay, it can be cut to a reasonable size or shredded, but the same food as the parents eat, with only a few exceptions. Which exceptions? Round, slippery food, such as whole grapes or peanuts are not a good idea. They are often just the size to block the baby’s trachea (breathing tube). Hot dogs present a similar risk. Popcorn has been cited as a food that can be aspirated into the trachea. Also very hot spicy food may be better to avoid for a while as burning the baby’s mouth is probably not a great way to encourage him to eat solids. But that’s about all. Of course, making sure the food is not too hot (in the sense of temperature) is just common sense and not only for babies or children. There’s often no need to cut the food into small pieces: a baby can hold a broccoli floret in his hand and gnaw away at it, or pick up a pear with two hands and chomp on it. But I have heard the argument that a baby of five or six months will put anything into his mouth, even stones and toys, if he has the opportunity. Yes, this is true and since the parents are usually there when a six month old baby is putting a plastic toy into his mouth, they will usually quickly and anxiously pull the toy out of his mouth. The baby has just learned that toys are not food or at least not to be put into the mouth though they will keep trying from time to time until they really learn. I would suggest, then, that if a baby puts a piece of chicken into his mouth and the parents react in the same way to the chicken as they would to the stone, the baby has just learned that maybe chicken is not food either. Excerpted from Facebook posts that were too good to lose:
Dr.Jack Newman- September 21 · I am concerned because I have received 2 emails in 2 days where a mother of a baby (in the second case a 9 month old) has been told that “breastfeeding causes iron deficiency”. Those words exactly. According to the mother of the 9 month old baby, the baby is eating meat at least once a day, sometimes twice a day and is eating iron fortified baby cereal in the morning. That the pediatrician would put it this way, that “breastfeeding causes iron deficiency” boggles the mind. And it worries me that I have received two similar emails in two days. I hope this is a coincidence and not a new trend based on some silly article or some talk at a conference by someone who knows nothing about breastfeeding toddlers or infant nutrition for that matter. In a way a pediatrician who says this is stating that formula is somehow better than breastfeeding. The pediatrician wanted the mother to breastfeed less frequently and give more frequent feedings of solids. As if solids somehow replace breastfeeding. Even though this 9 month old’s diet seems perfectly adequate from the point of view of his getting his requirements of iron. In fact, from all points of view. This pediatrician forgets (or never realized) that breastfeeding is much more than nutrition. Breastfeeding is not just another way of getting calories and other nutrients (including iron) into a baby. Breastfeeding is not just another way of feeding a baby with a “bottle” that is softer than plastic or glass bottles but essentially the same. Aside from the nutritional point of view, breastfeeding is chock full of many types of immune protective factors (not just antibodies) and growth factors (that help the baby’s gut, brain and other systems to develop) and even stem cells. But breastfeeding is also a relationship, a close, intimate relationship between two people in love. The question of iron deficiency has reached the point almost of hysteria, supported by formula companies who keep stressing to health professionals that one of the main reasons to give formula after the first 6 months is that it is a way of making sure that babies get enough iron. Which is ridiculous as the iron in formula is artificially added, so essentially it is really equivalent to giving babies medicinal iron. And the majority of the iron in formula (and baby cereals) ends up in the baby’s diaper. One of the most frequently cited reasons for starting babies on solids is that if they don´t start eating iron rich food they will become iron deficient and this is where the notion of "breastfeeding causes iron deficiency" comes in. This is further complicated by mothers being told to "replace breastfeeding with solids". What people need to understand is the following: 1) After the baby is six months of age, solids are ADDED to breastfeeding, they do not replace breastfeeding. 2) Breastmilk does contain iron and the iron in breastmilk is very well absorbed. So babies need the iron in breastmilk and addition iron in solids. 3) Breastfeeding shouldn't be replaced by formula after the first six months. The notion that formula needs to be introduced at some point in the baby's life is wrong. Breastfed babies eating solids don't need formula ever. 4) Breastmilk is still the main source of nutrition for babies after the first 6 months because it still contains all those hundreds of nutrients, cells and factors that it contained before. Dr.Jack Newman - September 24 · As a followup to the iron issue about which I posted here on September 21, the following is the abstract of an article that was published in the journal AMERICAN JOURNAL OF HUMAN BIOLOGY 26:10–17 (2014). It questions the basic assumption of what might be "normal" for the formula fed baby should be considered normal for the breastfed baby. Here is the abstract: Recently, there has been considerable debate regarding the appropriate amount of iron fortification for commercial infant formula. Globally, there is considerable variation in formula iron content, from 4 to 12 mg iron/L. However, how much fortification is necessary is unclear. Human milk is low in iron (0.2–0.5 mg/L), with the majority of infant iron stores accumulated during gestation. Over the first few months of life, these stores are depleted in breastfeeding infants. This decline has been previously largely perceived as pathological; it may be instead an adaptive mechanism to minimize iron availability to pathogens coinciding with complementary feeding. Many of the pathogens involved in infantile illnesses require iron for growth and replication. By reducing infant iron stores at the onset of complementary feeding, infant physiology may limit its availability to these pathogens, decreasing frequency and severity of infection. This adaptive strategy for iron regulation during development is undermined by the excess dietary iron commonly found in infant formula, both the iron that can be incorporated into the body and the excess iron that will be excreted in feces. Some of this excess iron may promote the growth of pathogenic, iron requiring bacteria disrupting synergistic microflora commonly found in breastfed infants. Evolutionarily, mothers who produced milk with less iron and infants who had decreased iron stores at the time of weaning may have been more likely to survive the transition to solid foods by having limited iron available for pathogens. Contemporary fortification practices may undermine these adaptive mechanisms and increase infant illness risk. Am. J. Hum. Biol. 26:10–17, 2014. VC 2013 Wiley Periodicals, Inc. Dr.Jack Newman - September 24, 2013 · The following is from a blog by a mother who tested her milk for alcohol. Not one of those useless kits that you can buy at various stores, but tested at a toxicology laboratory. I will copy from her blog the method she used and the results. I think this puts the lie to the notion that women should not drink while breastfeeding or need to "pump and dump" (an appalling term) after having even one drink. The following is an exact quote from her blog:
Method: First I took a sample of my milk (about 1 mL) prior to drinking any alcoholic beverage. I expressed the milk mid-nursing session to ensure I had a goodly portion of fore & hind milk. After completing the nursing session, I mixed myself an alcoholic beverage consisting of 2 oz of 80 proof (40%) vodka in 10 oz of soda (Sprite). I proceeded to drink the entire 12 oz in about 30 minutes. About 30 minutes after finishing (1 hour after beginning to drink), I expressed some milk (about 1 mL) and labeled it 'immediate'. I then waited 1 hour and expressed more milk (about 1 mL) and labeled it '2 hours'. In the 2 hours (from the beginning), I did not drink any more alcoholic beverages, drink other beverages, or eat any other foods. Another day, 1/2 of a beer (4.3% alcohol) and 2-6 oz glasses of wine were consumed within 1.5 hours. About an hour from the beginning of the last drink, a milk sample (about 1 mL) was taken. This sample was labeled '1 hour - 3 drinks'. Another sample was taken about an hour after that (2 hours after the beginning of the last drink). This sample was labeled '2 hours - 3 drinks'. The samples were stored in the refrigerator until processing. An Agilent headspace instrument was used to run the tests. Propanol and ethanol standards were also tested to ensure the instrument was within limits. The instrument is maintained by the KSP Lab Toxicology Section and used in forensic determinations of blood and urine alcohol content. Results: The sample labeled as 'immediate' registered as 0.1370 mg/mL which correlates to 0.01370% alcohol in the sample. The sample labeled '2 hours' registered as 0.0000 mg/ml which correlates to 0.0000%. The sample labeled '1 hour - 3 drinks' registered as 0.3749 mg/mL which correlates to 0.03749% alcohol in the sample. The sample labeled '2 hours - 3 drinks' registered as 0.0629 mg/mL which correlates to 0.00629% alcohol in the sample. Conclusion: The alcohol content in breast milk immediately after drinking is equivalent to a 0.0274 proof beverage. That's like mixing 1 oz of 80 proof vodka (one shot) with 2919 oz of mixer . By the way, 2919 oz is over 70 liters. Two hours after drinking one (strong) drink the alcohol has disappeared from the sample. Completely harmless to the nursing infant. Drinking about 3 drinks in 1.5 hours resulted in higher numbers, but still negligible amounts of alcohol would be transferred to the child. One hour after imbibing in 3 drinks, the milk was the equivalent of 0.07498 proof beverage. That would be like adding 1 oz of 80 proof vodka (one shot) to 1066 oz of mixer (1066 oz is over 26 liters). Two hours after imbibing in 3 drinks, the milk was 0.01258 proof. That would be like adding 1 oz of 80 proof vodka to 3179 oz of mixer (over almost 80 liters). So, even though an infant has much less body weight, any of these percentage of alcohol in breast milk is unlikely to adversely affect the baby. Bottoms up!
Below is a collection of the best advice the parents in our online support groups ever received. For your inspiration!
From The Womanly Art of Breastfeeding, 8th Edition by La Leche League International (c) 2011
The only thing I have to add to the above recommendations is to make the baby "work" for "letdown" while bottle feeding so that they have to suck that first stimulatory suck that they do when they latch onto the breast, which triggers the mother to let down. After a minute or so you can allow the nipple to get more milk to simulate letdown. After several minutes there, tilt the bottle backwards again so they have to "work" for another "letdown" and continue until the baby is finished (NOT necessarily until the bottle is empty). For folks who need some rules to follow- general rules of thumb include no more than once ounce per hour, and it's a good idea to have 20-30 minutes be the goal to finish the bottle. If the baby is finishing the bottle in less time than that, their stomachs won't have enough time to communicate to their brains that they're full. Slow feeds more accurately replicate breastfeeding so they prevent both overfeeding and flow preference! It's generally much better to offer smaller amounts more frequently (i.e. 1.5-2 ounces every 1.5-2 hours) than larger amounts less often (i.e. 3-4 ounces every 3-4 hours). I had a breast reduction in 2007 and was therefore told that I would not likely be able to breastfeed. During pregnancy, I was able to express some colostrum and was overcome with joy that there was a chance I would be successful! With flat and inverted nipples, latching in the beginning was difficult but I exclusively breastfed throughout my daughter’s first month, believing everything was fine.
At her 4 week checkup we discovered she had not yet regained her birth weight so I was given a can of formula by the pediatrician and a referral to a local IBCLC. I felt like the rug had been pulled from under me, so I began offering to nurse my daughter every 30-45 minutes, refusing to supplement if it was unnecessary. She happily nursed, however she had only gained a few ounces by the end of the week so I made an appointment with an IBCLC . After spending about 30 minutes with me the IBCLC diagnosed me with low supply as a result of my breast reduction and a single weigh-feed-weigh whereby my daughter took 1.5 ounces from my breasts. She recommended 3 ounce bottles of formula after every nursing session and that I rent a hospital grade pump and purchase a variety of galactagogues (including fenugreek) from the shop she worked for (totaling around $200 when everything was said and done!). From there I began pumping after every nursing session and supplementing with formula by bottle as I was told, and within 2 weeks my daughter was refusing to nurse altogether- in fact, if she even saw my breasts she would start screaming. At this point I did two things; I joined Diana West’s BFAR fora and began learning about supplemental nursing systems and galactagogues that would actually be helpful to me. I also began seeking donor milk for my daughter so that I could get her off of formula. I began researching fenugreek and learned that it is actually unsafe for me to take (with my food allergies and hypothyroidism) and I scheduled an appointment with the Newman Breastfeeding Clinic and Institute in Toronto. I also ordered some domperidone online and had a discussion with my primary doctor (PLEASE never begin any medication/supplement without first discussing it with your medical care provider AND your IBCLC), who could not see any reason why it might be harmful for me, and I started myself on the middle recommended dose per Dr. Newman's instructions. Within 24 hours I was engorged and my pumping output was increasing. I began slowly using a Madela SNS I purchased to help combat the flow preference I saw my daughter had developed. I was still “power pumping” with my rented Madela Symphony every 2-3 hours for 15-30 minutes on a 24/7 basis and soon I found that I was able to stop relying on donated milk, being able to pump 1.5-2 ounces during each nursing session. Along the way I also noticed that my daughter couldn’t stick her tongue out very far, so I scheduled an appointment with an ENT per my pediatrician’s recommendation to get her evaluated for a tongue tie. It was confirmed and her tie was snipped, but it was still very slow going getting her back to the breast and she still received bottles for most of her meals. After her tongue tie release I had her latch re-evaluated by a La Leche League leader in my area, and she confirmed that the latch looked good and was deep, but I noticed that over the next week or two she had started making some clicking noises as she suckled. I read that it was common for there to be loss of suction or clicking sorts of noises as a baby got used to using an un-tied tongue, so I didn’t worry about it. Time came for my appointment at the Newman Clinic and by then I was so stressed out that my supply had actually plummeted (despite being on 120mg of domperidone and power pumping) and at the appointment I was unable to get even one let down. I was fortunate to be able to see Edith Kernerman (co-founder of the Newman Clinic), who recommended that I increase my domperidone dosage to 160/day and that if supplementation was necessary and I couldn’t get donor milk or my own supply up adequately, that solids may be introduced prior to 6 months as a healthier alternative to formula. She also pointed out that my daughter was still tongue tied, and that less than 2 weeks following her tongue tie release it hadn’t been snipped enough- they left a posterior tie in her mouth, and she showed me how to spot posterior ties as opposed to the more typical ties. After my appointment at the clinic I was disheartened and accepted the fact that I’d be in this cycle forever. I scheduled another appointment for a second frenectomy and had to argue with the doctor in order to get it done (he was refusing and telling me that I "didn't have to put her through this again when formula is a perfectly good option"). Claudia was just starting to nurse more often as I increased my domperidone dosage and I started giving fewer bottles. I used the largest tubing in the SNS and raised the container high above her head for the fastest flow possible, while giving slow flow bottles and only giving a small amount at a time. I was trying to get her to reverse her flow preference to ME instead of to the bottles. It started working! It got to a point where I was able to pump 1.5 ounces after every feeding, and then I was giving those 1.5 ounces back to her via the SNS at the next feeding. At this point I began lowering the tube size and restricting the flow of milk she got, and clamping the tubes for incrementally longer periods of time so that she would have to wait for “letdown” before she got milk. At 5.5 weeks I saw an IBCLC. By 8 weeks my daughter was no longer nursing. By 10 weeks we obtained our SNS. Around 12 weeks I found her tongue tie and by 14 she had her first frenectomy. At 16 weeks we went to NBCI and by 18 she had her second frenectomy. By 20 weeks we were finally exclusively breastfeeding again with no pump, no SNS, and no supplementation! At that point I weaned down from the domperidone (per Dr. Newman's dosing instructions) until we finally had a normal breastfeeding relationship (just in time to start introducing solids lol). It was a long road, but I’d do it all again in a heartbeat because now our nursing relationship is as strong as ever. I do feel extremely frustrated, however, because had her tongue tie been seen in the beginning, I would not have endured so many months of struggle and heartache… but had I not experienced any of it I would not have found myself in the amazing position I’m in today of being able to help so many mothers with their own issues, having learned so much from mine! |
AboutHere is our database of resources as well as food for thought! Archives
April 2021
Categories
All
|
HO*LIS*TIC ~ADJECTIVE: Relating to or concerned with complete systems rather than with individual parts
WNY Orofacial & Breastfeeding Support Center is a division of Holistic Parenting Network, LLC, located within the village of East Aurora, NY.
131 Orchard Park Rd. West Seneca, NY 14224 fax: (716) 508-3302 (716) 780-2662 [text friendly]
WNY Orofacial & Breastfeeding Support Center is a division of Holistic Parenting Network, LLC, located within the village of East Aurora, NY.
131 Orchard Park Rd. West Seneca, NY 14224 fax: (716) 508-3302 (716) 780-2662 [text friendly]
 RSS Feed
RSS Feed